What are sleep disorders?
Sleep disorders are medical conditions that interfere with a person’s ability to achieve regular, restful sleep. These disturbances can manifest as difficulty falling asleep, staying asleep, or waking too early and being unable to return to sleep. Individuals experiencing persistent sleep issues often suffer from excessive daytime fatigue, irritability, reduced concentration, and impaired daily functioning.
According to the National Heart, Lung, and Blood Institute, sleep disorders affect an estimated 50 to 70 million adults in the United States, with conditions ranging in severity from occasional disturbances to chronic, life-altering disorders such as insomnia and obstructive sleep apnea. You can read more about this from their official page: NHLBI - Sleep Deprivation and Deficiency.
Sleep plays a critical role in supporting your body’s physical health and mental well-being. During restorative sleep, vital processes such as memory consolidation, tissue repair, and immune system strengthening occur. Chronic sleep disruption can impair these functions and increase the risk of health issues such as obesity, cardiovascular disease, diabetes, and depression.
Why Is It Important to Understand Sleep Disorders?
Understanding sleep disorders is crucial for several reasons, as untreated sleep issues can have a profound impact on both physical and mental health. Poor sleep quality affects not just sleep onset but also the duration and depth of sleep. As a result, it can lead to daytime fatigue, increased drowsiness, and more severe conditions such as high blood pressure, diabetes, and heart disease. Studies published by the National Institutes of Health (NIH) show that chronic sleep deprivation is linked to the development of various cardiovascular issues and metabolic disorders. For further reading, you can check out the NIH’s official guide on sleep and heart health.
Moreover, understanding sleep disorders allows individuals to recognize when their sleep disturbances are not just temporary issues but symptoms of underlying conditions that require professional treatment. According to the American Academy of Sleep Medicine (AASM), conditions such as insomnia, sleep apnea, and narcolepsy should be diagnosed and managed promptly to prevent long-term health complications. More details about the importance of diagnosing and treating these disorders can be found in their resource on sleep disorders and treatment.
For parents, understanding sleep disorders in children is especially important. Conditions like sleepwalking, night terrors, and restless leg syndrome may disrupt sleep, but they can also lead to physical injuries or emotional distress for both the child and their family. Early intervention and treatment can mitigate these risks, improving both the child’s sleep quality and overall well-being.

Types of Sleep Disorders
Sleep disorders affect millions worldwide, profoundly impacting physical health, cognitive function, and quality of life. According to the Centers for Disease Control and Prevention (CDC), approximately 50-70 million adults in the United States suffer from chronic sleep or wakefulness disorders. These disorders range from difficulties in falling asleep to severe interruptions in breathing during sleep, leading to increased risks of cardiovascular diseases, metabolic disorders, and mental health conditions. Below is a comprehensive overview of the most common sleep disorders, with detailed scientific insights and prevalence data.
Insomnia
Insomnia is the most prevalent sleep disorder, affecting an estimated 10-30% of adults globally. It is characterized by difficulty initiating or maintaining sleep or experiencing non-restorative sleep, despite adequate opportunity to sleep. Chronic insomnia, defined as symptoms lasting more than three months, affects about 10-15% of the adult population. Insomnia significantly increases the risk of depression and anxiety, with studies showing a 2- to 5-fold increased risk of developing these disorders in individuals suffering from persistent insomnia. Furthermore, insomnia-related fatigue impairs cognitive performance, reducing attention, memory, and executive function. The disorder can be precipitated by stress, lifestyle factors, or comorbid medical conditions such as chronic pain or cardiovascular disease. Cognitive Behavioral Therapy for Insomnia (CBT-I) remains the first-line evidence-based treatment, with response rates exceeding 70%, often outperforming pharmacological interventions in the long term.
Sleep Apnea
Sleep apnea, particularly Obstructive Sleep Apnea (OSA), affects approximately 9-38% of the adult population, with higher prevalence in males and obese individuals. OSA involves repeated episodes of partial or complete upper airway obstruction during sleep, leading to intermittent hypoxia and sleep fragmentation. It is estimated that nearly 80% of moderate to severe OSA cases remain undiagnosed. Symptoms include loud snoring, witnessed apnea, gasping during sleep, and excessive daytime sleepiness. OSA is strongly associated with hypertension, atrial fibrillation, stroke, and insulin resistance. The Sleep Heart Health Study demonstrated a 2- to 3-fold increased risk of cardiovascular events in individuals with severe OSA. Continuous Positive Airway Pressure (CPAP) therapy is the gold standard treatment and has been shown to reduce cardiovascular morbidity by improving oxygenation and reducing sympathetic nervous system activation.
Narcolepsy
Narcolepsy is a rare but debilitating neurological disorder characterized by excessive daytime sleepiness, affecting about 0.02-0.05% of the population. It typically manifests in adolescence or early adulthood. Patients experience sudden, irresistible sleep attacks and often cataplexy, a sudden loss of muscle tone triggered by strong emotions, occurring in up to 70% of cases. Narcolepsy results from the loss of hypothalamic neurons producing hypocretin (orexin), a neuropeptide critical for maintaining wakefulness. This loss leads to dysregulation of REM sleep, causing symptoms like sleep paralysis and hypnagogic hallucinations. Diagnosis is confirmed by polysomnography and the Multiple Sleep Latency Test (MSLT). Although incurable, pharmacological treatments such as modafinil and sodium oxybate improve wakefulness and quality of life.
Restless Leg Syndrome (RLS)
Restless leg syndrome affects about 5-10% of adults in the United States and Europe, with a higher prevalence in women and older adults. RLS is characterized by an uncontrollable urge to move the legs, often accompanied by uncomfortable sensations described as crawling, tingling, or burning. These symptoms predominantly worsen during rest or at night, leading to prolonged sleep latency and fragmentation. The pathophysiology is linked to dysfunction in the dopaminergic system and brain iron metabolism. RLS frequently coexists with periodic limb movement disorder (PLMD), which affects up to 80% of RLS patients. Treatment includes dopamine agonists and iron supplementation where deficiency is identified. Left untreated, RLS significantly impairs quality of life and is associated with increased cardiovascular risk.
REM Sleep Behavior Disorder (RBD)
REM sleep behavior disorder is a parasomnia characterized by the loss of normal muscle atonia during REM sleep, resulting in individuals physically acting out vivid dreams. RBD affects approximately 0.5% of the general population, with prevalence increasing with age, especially after 60. It is strongly associated with neurodegenerative diseases such as Parkinson’s disease and Lewy body dementia; longitudinal studies show that over 80% of idiopathic RBD patients develop Parkinsonism within 10-15 years. Clinical presentation includes violent movements that can lead to injury. Diagnosis is confirmed by polysomnography showing REM sleep without atonia. Early diagnosis is crucial, as RBD serves as a prodromal marker for synucleinopathies, allowing for closer neurological monitoring.
Circadian Rhythm Disorders
Circadian rhythm disorders occur when the internal biological clock is misaligned with environmental cues, leading to impaired sleep timing. Delayed Sleep Phase Disorder (DSPD) is the most common subtype, affecting up to 7-16% of adolescents and young adults, characterized by difficulty falling asleep until very late at night. Advanced Sleep Phase Disorder (ASPD) is less common, typically affecting older adults who fall asleep and wake earlier than desired. Shift Work Disorder affects approximately 10-40% of shift workers, resulting in insomnia and excessive sleepiness. These disorders disrupt melatonin secretion and core body temperature rhythms, impairing restorative sleep and increasing risks for metabolic syndrome and mood disorders.
Sleepwalking (Somnambulism)
Sleepwalking is a complex motor behavior arising during slow-wave non-REM sleep, affecting 1-15% of children and 1-4% of adults. Episodes range from sitting up in bed to walking and performing routine tasks, often with no memory of the event. Sleepwalking has a strong genetic component, with increased incidence in families. It is precipitated by sleep deprivation, stress, and certain medications. While mostly benign, it can lead to injury or dangerous behavior. Treatment focuses on safety measures and managing triggers; pharmacotherapy is rarely required.
Sleep Paralysis
Sleep paralysis is a transient inability to move or speak during the transition between wakefulness and sleep, affecting up to 8% of the general population. It is often accompanied by vivid hallucinations and a sensation of chest pressure. Sleep paralysis is associated with sleep deprivation, irregular sleep schedules, and narcolepsy. Though typically benign, recurrent episodes may cause significant anxiety.
Hypersomnia
Hypersomnia is characterized by excessive daytime sleepiness despite adequate or prolonged nighttime sleep. It affects approximately 5% of the population and can result from conditions such as idiopathic hypersomnia, sleep apnea, and depression. It is diagnosed via polysomnography and Multiple Sleep Latency Test. Untreated hypersomnia impairs cognitive function, mood, and daily functioning.
Parasomnias
Parasomnias encompass abnormal behaviors during sleep, including night terrors, sleepwalking, and bruxism. Night terrors occur mostly in children and involve abrupt awakenings with intense fear and autonomic activation. Bruxism affects approximately 8-31% of the population and can cause significant dental wear and pain. Parasomnias often disrupt sleep continuity and may require behavioral or pharmacological treatment.
Bruxism (Teeth Grinding)
Bruxism is a repetitive jaw-muscle activity characterized by clenching or grinding of the teeth during sleep. Prevalence is estimated at 8-31% in adults. It is linked to stress, anxiety, and sleep disorders such as OSA. Untreated bruxism can cause temporomandibular joint dysfunction and dental damage. Management includes dental guards, stress reduction, and treating underlying disorders.
Night Terrors
Night terrors affect up to 6% of children and less than 1% of adults. These episodes occur during deep non-REM sleep and involve sudden arousal with intense fear, screaming, and autonomic symptoms. Unlike nightmares, individuals usually do not remember night terrors. They are typically benign but can be distressing and disrupt sleep.
Hypnic Jerks
Hypnic jerks are sudden, involuntary muscle twitches occurring at sleep onset, experienced by up to 70% of people. They are usually harmless but can cause brief awakenings and frustration in falling asleep.
Sleep-Related Eating Disorder (SRED)
Sleep-related eating disorder involves episodes of compulsive eating during partial arousals from sleep, often with impaired awareness. Prevalence is rare but increases in individuals with other sleep disorders such as RLS and parasomnias. It poses risks of weight gain and metabolic disturbances.
Periodic Limb Movement Disorder (PLMD)
Periodic limb movement disorder is characterized by repetitive, involuntary limb movements during sleep, affecting 4-11% of adults. These movements cause sleep fragmentation and daytime sleepiness, often coexisting with RLS.
Nocturia
Nocturia is the need to wake during the night to urinate, affecting over 50% of adults older than 60. It leads to disrupted sleep and increased risk of falls, depression, and reduced quality of life. Causes include bladder dysfunction, diabetes, and heart disease.
Causes of Sleep Disorders
Sleep disorders arise from a complex interplay of genetic, environmental, lifestyle, and medical factors. Understanding these causes can facilitate early diagnosis, targeted treatment, and effective prevention strategies.
Genetics
Genetic predisposition plays a significant role in many sleep disorders. For instance, narcolepsy exhibits familial clustering, with first-degree relatives having a 1-2% risk compared to 0.02-0.05% in the general population. Specific genetic markers, such as the HLA-DQB1*06:02 allele, are strongly associated with narcolepsy, implicating immune system dysfunction. Similarly, restless leg syndrome (RLS) demonstrates a hereditary pattern, with genome-wide association studies identifying multiple risk loci affecting dopamine pathways and iron metabolism. Approximately 40-60% of individuals with RLS report a family history, suggesting a strong genetic influence. Recognizing these genetic factors enables clinicians to identify at-risk individuals and consider early interventions.
Environmental Factors
External environmental influences significantly impact sleep quality and can trigger or worsen sleep disorders. Common environmental disruptors include noise pollution, light exposure, and thermal discomfort. Chronic exposure to nighttime noise above 55 decibels is linked to increased awakenings and reduced slow-wave sleep. Light pollution, especially exposure to blue light from screens, suppresses melatonin secretion, a hormone crucial for regulating circadian rhythms. Studies show that even low levels of artificial light at night can delay sleep onset by up to 90 minutes. Furthermore, an uncomfortable sleep environment—due to factors like inappropriate room temperature or an unsupportive mattress—negatively affects sleep architecture. Implementing good sleep hygiene practices, such as minimizing noise and light and optimizing bedroom conditions, is proven to reduce sleep disturbances.
Lifestyle Choices
Lifestyle factors are among the most modifiable contributors to sleep disorders. Irregular sleep schedules, common in shift workers and those with high social jetlag, disrupt circadian synchronization, leading to conditions like shift work disorder. Excessive consumption of caffeine (more than 400 mg daily) delays sleep onset and reduces total sleep time by blocking adenosine receptors. Chronic stress elevates cortisol levels, which inhibits melatonin production and hampers the ability to fall asleep. Physical inactivity and poor diet also negatively impact sleep quality; conversely, regular exercise improves sleep latency and efficiency. A meta-analysis of 66 studies confirmed that moderate aerobic exercise reduces symptoms of chronic insomnia by 47%, highlighting lifestyle modification as a powerful therapeutic tool.
Medical Conditions
Numerous medical disorders increase the risk or severity of sleep disturbances. OSA’s intermittent hypoxia exacerbates hypertension, increasing cardiovascular morbidity. Neurological diseases such as Parkinson's disease and multiple sclerosis disrupt sleep regulation centers, leading to insomnia, REM sleep behavior disorder, and excessive daytime sleepiness. Additionally, chronic pain conditions, gastroesophageal reflux disease (GERD), and psychiatric illnesses such as depression and anxiety are commonly associated with poor sleep. Management of underlying medical conditions is often essential for improving sleep quality and reducing comorbid sleep disorders.
Light Therapy for Sleep Disorders
How Light Therapy Works
Light therapy is a scientifically recognized treatment that plays a crucial role in managing circadian rhythm disorders and enhancing sleep quality. This therapy involves exposure to bright light at specific times of the day, typically during the morning hours, to help reset the body’s internal clock, known as the circadian rhythm. This rhythm regulates sleep-wake cycles, body temperature, hormone release, and other physiological processes over a 24-hour period. Disruptions to the circadian rhythm can lead to sleep disturbances, contributing to conditions such as insomnia, winter blues, jet lag, and shift work sleep disorder. For an in-depth explanation, see how light therapy works.
The effect of light on our circadian rhythm is backed by decades of research. Studies have shown that exposure to bright light in the morning helps synchronize the biological clock, especially in individuals suffering from circadian misalignment. A study conducted in 2018 demonstrated that light exposure in the morning significantly improved the sleep onset and overall sleep quality for those with delayed sleep phase disorder (a type of circadian rhythm disorder) by up to 60%.
Furthermore, light therapy also influences melatonin production, a hormone that helps regulate sleep and wakefulness. When exposed to bright light, especially in the morning, melatonin production is suppressed, signaling the body to stay alert. Conversely, reduced light exposure in the evening increases melatonin levels, preparing the body for sleep. This balancing act between light exposure and melatonin secretion forms the foundation of light therapy's efficacy. For more on light's effects on hormones, check this article.
Benefits of Light Therapy
The primary benefit of light therapy lies in its ability to regulate melatonin production and align the circadian rhythm with external environmental cues. Research has consistently shown that light therapy can significantly improve sleep onset, sleep duration, and overall sleep quality. It is particularly effective for individuals whose internal body clock is misaligned, such as shift workers, frequent travelers, or people experiencing seasonal mood swings. Learn more about light therapy for sleep.
A clinical study conducted in 2007 by the National Institute of Mental Health found that light therapy reduced symptoms of Seasonal Affective Disorder (SAD), which affects about 5% of the U.S. population annually, particularly in the winter months when daylight hours are shorter. The study showed that exposure to bright light for 30 to 45 minutes each morning could alleviate depressive symptoms associated with SAD by 50-60%. Similarly, shift workers—whose work hours often conflict with their natural circadian rhythms—benefit from light therapy, as it helps re-align their sleep-wake cycle to a more natural rhythm, reducing the risk of sleep disorders and improving overall health. You can read more in the night working light therapy guide.
Additionally, light therapy has been shown to be an effective treatment for jet lag, a condition commonly experienced by individuals traveling across multiple time zones. A 2016 study published in the "Journal of Clinical Sleep Medicine" found that light exposure timed to the destination's local time zone significantly reduced jet lag symptoms, improving sleep quality and daytime alertness within a few days of travel. Learn how light helps with jet lag symptoms.
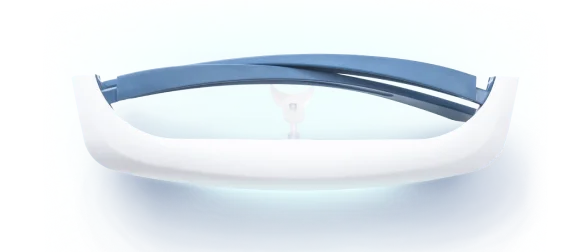
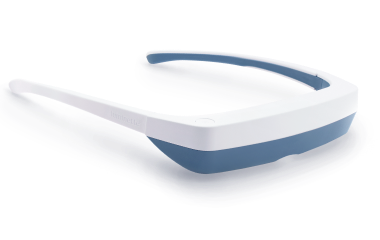
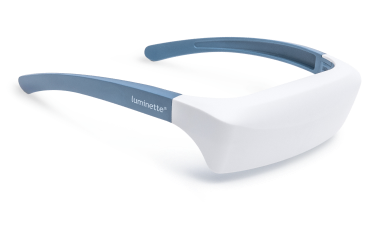
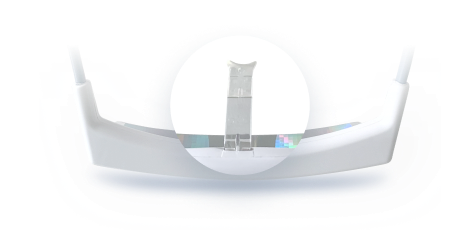
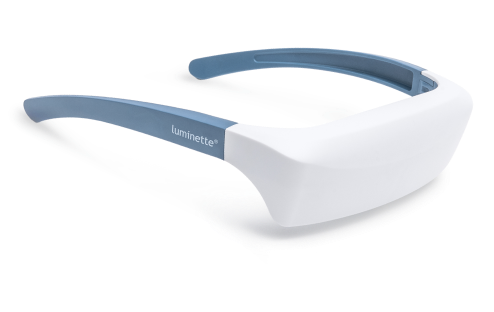
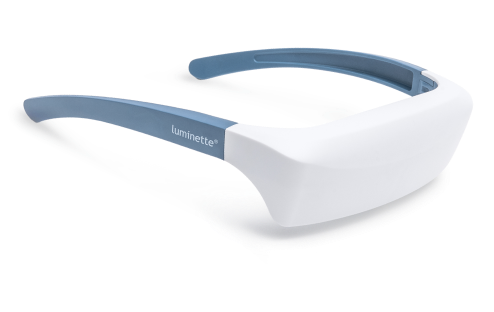
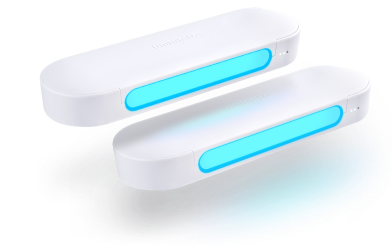
Luminette and Its Role in Light Therapy
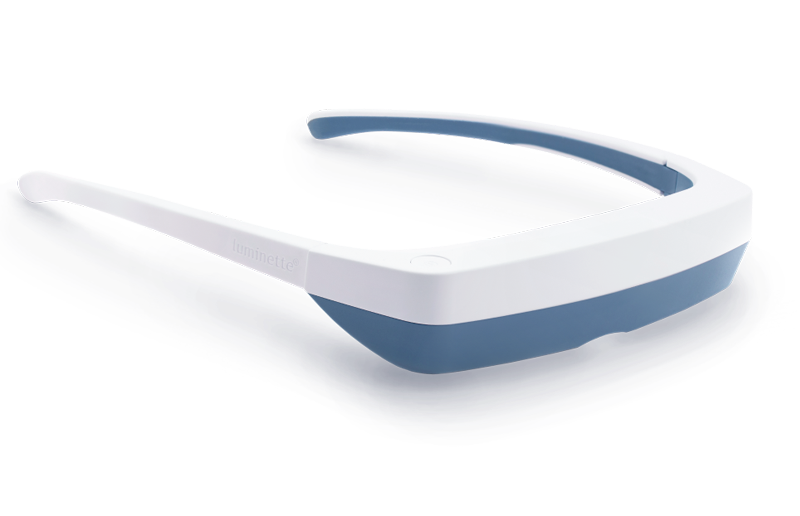
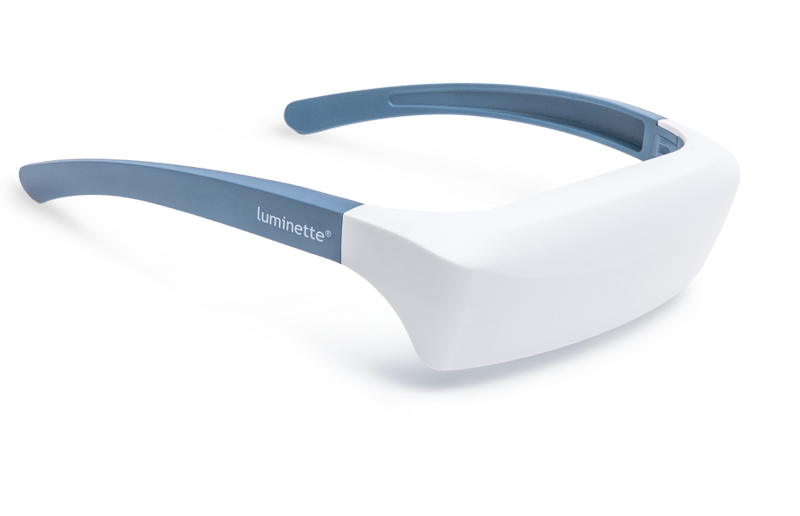
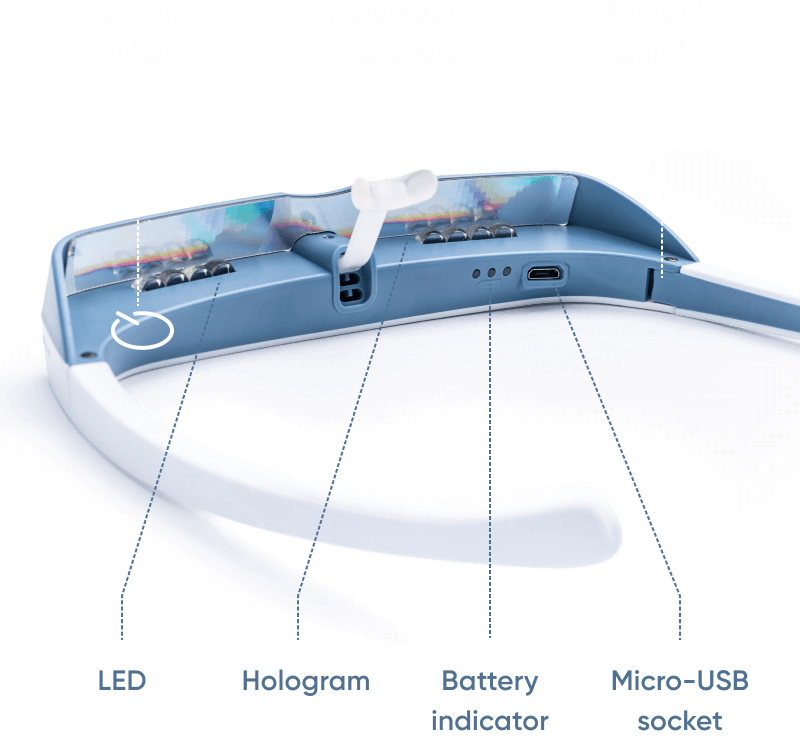
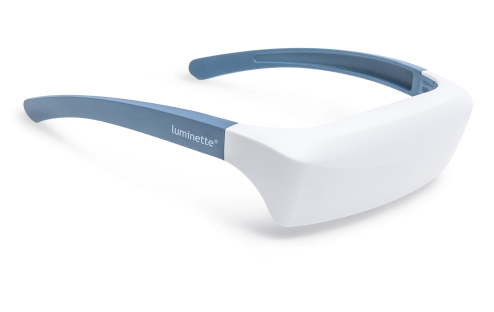
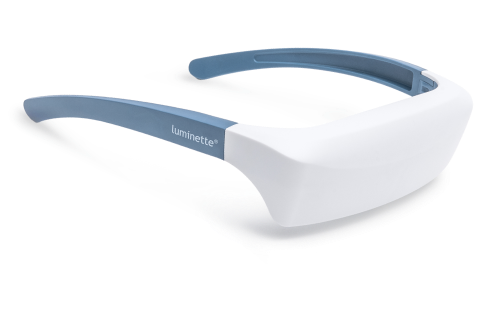
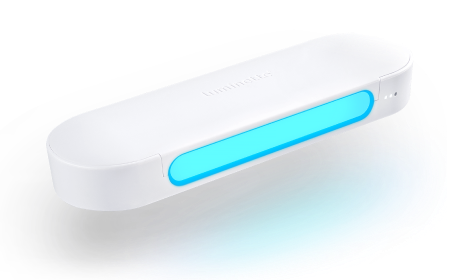
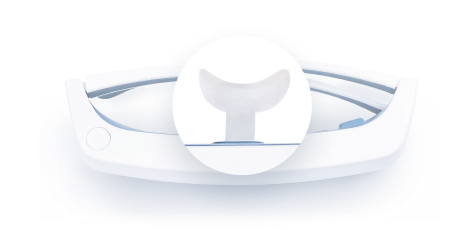
One of the innovative devices designed to deliver light therapy in a convenient and effective manner is the Luminette 3. The Luminette is a portable, wearable light therapy device that provides targeted exposure to bright, high-quality light. Unlike traditional light therapy boxes, which often require users to sit in front of a stationary device for extended periods, the Luminette offers a more flexible and user-friendly approach. Its wearable design allows users to go about their daily activities while receiving the benefits of light therapy, making it ideal for people with busy schedules.
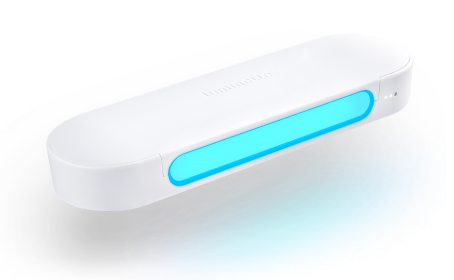
The Luminette has been shown to be particularly effective for individuals with circadian rhythm disorders, such as shift work sleep disorder and delayed sleep phase disorder. The device is based on the principles of light therapy and is designed to provide the optimal wavelength of light needed to influence the circadian rhythm. It emits blue-enriched white light at an intensity of 10,000 lux, the recommended level for effective treatment of circadian rhythm disturbances. Some research indicates that exposure to blue light during the morning hours can significantly improve sleep onset, sleep quality, and daytime alertness by enhancing melatonin suppression and regulating the sleep-wake cycle. You can explore more in Luminette vs. other brands or learn about the science behind blue light therapy benefits.
Moreover, the Luminette is user-friendly and convenient. Its compact size and ease of use make it a preferred choice for individuals seeking a portable solution to address their sleep disorders. Since it does not require a stationary setup, users can engage in various tasks, such as reading, working, or commuting, while benefiting from the therapeutic light exposure. This level of convenience is crucial for individuals with demanding work schedules or those who travel frequently and need to adjust their internal clocks rapidly. Learn how to get the best results from light therapy usage tips.
Treatment Options for Sleep Disorders
Cognitive Behavioral Therapy for Insomnia (CBT-I)
Cognitive Behavioral Therapy for Insomnia (CBT-I) is one of the most well-researched and effective treatments for chronic insomnia. Unlike medication-based treatments, CBT-I targets the root causes of insomnia by focusing on the psychological and behavioral factors that contribute to sleep disturbances. This therapy is based on the premise that negative thoughts and unhealthy sleep habits can perpetuate sleep problems, creating a vicious cycle of poor sleep and increased anxiety about sleep. By breaking this cycle, CBT-I helps individuals develop healthier sleep patterns and achieve long-lasting improvements in their sleep quality.
CBT-I involves several components, including cognitive restructuring, sleep restriction, and stimulus control. Cognitive restructuring helps individuals identify and challenge negative thoughts and beliefs about sleep, such as the fear that not getting enough sleep will lead to poor performance the next day. Through sleep restriction, the amount of time spent in bed is gradually limited to match the actual amount of sleep, which helps individuals consolidate their sleep and reduce the time spent lying awake. Stimulus control involves changing behaviors that are associated with wakefulness, such as avoiding using the bed for activities like watching TV or using electronic devices.
Research has shown that CBT-I can significantly reduce sleep onset latency (the time it takes to fall asleep), increase sleep efficiency, and improve sleep quality in individuals with chronic insomnia. A meta-analysis published in 2015 in the American Journal of Psychiatry found that CBT-I was highly effective in treating insomnia, with about 70-80% of individuals experiencing significant improvements in their sleep patterns. Additionally, the effects of CBT-I tend to last long after the therapy has been completed, making it one of the most sustainable treatment options for insomnia. More information about CBT-I can be found at the Mayo Clinic.
Medications
While behavioral interventions like CBT-I are often the first line of treatment for sleep disorders, pharmacotherapy can also be an important component of a comprehensive treatment plan. Medications may be used when other interventions have not been effective or when sleep disorders are caused by underlying conditions such as anxiety, depression, or obstructive sleep apnea. Medications may include sedatives, sleep aids, and antidepressants, among others, and are typically used for short-term management of sleep problems.
Sedatives work by enhancing the effects of the neurotransmitter gamma-aminobutyric acid (GABA), which inhibits brain activity and promotes relaxation. These medications are effective in helping individuals fall asleep more easily, but they come with risks of tolerance, dependence, and side effects such as memory problems and daytime drowsiness.
For individuals with chronic insomnia related to anxiety or depression, antidepressants may be prescribed. Certain types of antidepressants have sedating properties that can help improve sleep.
Melatonin receptor agonists mimic the action of melatonin, a hormone that helps regulate the sleep-wake cycle. These medications are particularly useful for individuals with circadian rhythm disorders, such as delayed sleep phase disorder, as they help reset the internal body clock. More about medications for sleep disorders can be explored on the Sleep Foundation's sleep hygiene page.
Lifestyle Changes
Lifestyle changes are often the first and most crucial step in managing sleep disorders. Improving sleep hygiene—the habits and practices that promote consistent, restful sleep—is key to restoring the body’s natural sleep-wake cycle. These changes can be easily implemented and can significantly improve sleep quality over time.
One of the most important aspects of sleep hygiene is maintaining a consistent sleep schedule. Going to bed and waking up at the same time every day, even on weekends, helps regulate the body’s circadian rhythms, making it easier to fall asleep and wake up naturally. Irregular sleep patterns, such as staying up late or sleeping in on weekends, can disrupt the internal clock and contribute to sleep deprivation and daytime fatigue.
Creating a comfortable sleep environment is another important factor in improving sleep quality. This includes ensuring the bedroom is cool, quiet, and dark, as these conditions are conducive to restorative sleep. The use of blackout curtains or sleep masks can block out ambient light, while earplugs or white noise machines can help mask disruptive noises. It is also important to choose a comfortable mattress and pillow that support a restful night’s sleep.
Avoiding stimulants like caffeine, nicotine, and alcohol before bedtime is another key lifestyle change. These substances can interfere with the body’s ability to fall asleep and stay asleep. Caffeine, for example, has a half-life of about 5-6 hours, meaning that consuming it in the late afternoon or evening can disrupt sleep even hours after ingestion. Similarly, alcohol, while initially sedating, can lead to fragmented sleep and frequent awakenings during the night.
In addition to these practical changes, managing stress through relaxation techniques can also improve sleep hygiene. Practices such as deep breathing, progressive muscle relaxation, and meditation can help calm the mind and prepare the body for sleep. Incorporating regular physical activity into the daily routine—preferably earlier in the day—can also help promote better sleep, as exercise has been shown to improve both sleep onset and sleep quality. More details on how exercise benefits sleep are available in the Sleep Foundation's exercise and sleep article.
Light Therapy
For individuals with circadian rhythm disorders, light therapy is one of the most effective tools for regulating sleep and improving sleep quality. Circadian rhythm disorders occur when the body’s internal clock is misaligned with external environmental cues, such as the sleep-wake cycle. Conditions like delayed sleep phase or shift work sleep problems and winter blues are common examples of circadian rhythm disorders that can lead to significant sleep disturbances.
Light therapy works by exposing the individual to bright light at specific times of the day, usually in the morning, to help reset the body’s internal clock. The most effective light for this purpose is bright, white light with an intensity of about 10,000 lux, which is about 20 times brighter than typical indoor lighting. Light exposure in the morning, when the body’s natural circadian rhythm is most sensitive to light, helps advance the sleep-wake cycle, making it easier to fall asleep at a desired bedtime and wake up in the morning.
For individuals dealing with shift work or jet lag, light therapy can be particularly beneficial. A study published in 2002 in the American Journal of Physiology found that light therapy was effective in reducing the symptoms of jet lag, with participants reporting improved sleep quality and daytime alertness after just a few days of light exposure. For shift workers, light therapy can help adjust the body’s internal clock to align with their work schedule, reducing the negative impact of irregular sleep patterns.
Devices such as the Luminette, a wearable light therapy device, allow individuals to receive light therapy while going about their daily activities. This can be particularly convenient for people who may not have the time to sit in front of a stationary light box for the recommended 30-45 minutes each day. The Luminette emits bright, targeted light that can be used during activities like reading, commuting, or working, providing a practical solution for those with busy lifestyles
Preventive Measures for Sleep Disorders
Creating a Sleep-Friendly Environment
A sleep-friendly environment is one of the most important preventive measures to ensure restorative sleep and overall well-being. The environment in which you sleep significantly impacts the quality and duration of your rest. Research has shown that individuals who create an optimal sleep environment tend to experience deeper sleep and wake up feeling more refreshed and alert.
The first step in creating a sleep-friendly environment is ensuring that your bedroom is dark. Light exposure during the night can disrupt the body’s circadian rhythm and hinder the production of melatonin, a hormone that regulates the sleep-wake cycle. Even small amounts of light, such as from streetlights or electronic devices, can interfere with sleep. According to a study published in Sleep Health (2015), light exposure at night, even from artificial sources, can delay sleep onset and reduce sleep quality. To minimize light exposure, consider using blackout curtains, sleep masks, or turning off any unnecessary lights before going to bed.
Noise is another factor that can disrupt sleep onset and prevent a restful night’s sleep. Even low levels of noise, such as a ticking clock or traffic outside, can interrupt deep sleep stages. A study conducted by the American Sleep Association in 2014 found that chronic exposure to environmental noise, especially at night, is associated with poor sleep quality and increased stress levels. To mitigate this, consider using earplugs, a white noise machine, or a fan to block out background sounds.
The temperature of your bedroom also plays a significant role in promoting restorative sleep. The body’s core temperature naturally drops during sleep, signaling that it’s time to rest. A cooler room (between 60°F and 67°F, or 15°C and 20°C) promotes this decline in body temperature, facilitating a more comfortable sleep. A study published in the Journal of Sleep Research in 2009 confirmed that cooler temperatures improve sleep efficiency and reduce nighttime awakenings.
Additionally, removing distractions like electronic devices from the bedroom is crucial for maintaining a sleep-friendly environment. The blue light emitted from smartphones, tablets, and laptops has been shown to suppress melatonin production, delaying sleep onset. According to a study by the Harvard Medical School in 2012, the blue light emitted by screens can disrupt sleep if used too close to bedtime. To minimize the impact, consider keeping electronics out of the bedroom or using settings that reduce blue light exposure in the evening.
Maintaining a Regular Sleep Schedule
One of the most effective ways to prevent sleep disorders is by maintaining a regular sleep schedule. The body’s internal clock, also known as the circadian rhythm, functions best when it is aligned with external environmental cues like light and dark. Going to bed and waking up at the same time every day, even on weekends, can help regulate the sleep-wake cycle and improve overall sleep quality.
A consistent sleep schedule ensures that the body gets the appropriate amount of sleep at the right times, promoting natural melatonin production and optimizing sleep efficiency. When the sleep-wake cycle is disrupted—such as through irregular sleep patterns or inconsistent bedtimes—it can cause sleep difficulties and contribute to the development of sleep disorders like insomnia. A 2014 study published in Sleep Medicine Reviews found that irregular sleep schedules were linked to poorer sleep quality and increased daytime fatigue.
Even small fluctuations in your sleep schedule, such as staying up late on weekends, can lead to sleep deprivation and negatively affect your ability to fall asleep during the week. This phenomenon is commonly referred to as “social jetlag,” and it can disrupt both your internal clock and sleep patterns. A study conducted by the Sleep Research Society in 2017 demonstrated that even one hour of variation in sleep schedule per night could lead to significant disturbances in sleep quality and daytime performance.
To maintain a consistent sleep schedule, aim to go to bed and wake up at the same time each day, including weekends. It may take some time to adjust your body to a new routine, but over time, your body will adapt, and you will find it easier to fall asleep and wake up naturally. If you need to adjust your schedule, try shifting your sleep time by 15 to 30 minutes each day until you reach your desired bedtime.
Reducing Stress
Chronic stress is one of the most significant contributors to sleep disorders. When the body is under stress, the sympathetic nervous system is activated, causing an increase in the production of stress hormones like cortisol. High levels of cortisol, especially in the evening, can interfere with the body’s ability to relax and initiate sleep. According to a 2013 study published in Psychosomatic Medicine, elevated cortisol levels are associated with poor sleep quality and difficulty falling asleep.
Relaxation techniques are some of the most effective ways to reduce stress and improve sleep. Activities like deep breathing, meditation, and yoga help activate the parasympathetic nervous system, which counteracts the effects of stress and promotes relaxation. A 2016 study in Journal of Clinical Psychology demonstrated that deep breathing exercises significantly reduced anxiety and improved sleep onset for individuals with chronic insomnia.
Incorporating relaxation techniques into your bedtime routine can also help signal to the body that it is time to wind down. Practices such as progressive muscle relaxation, which involves tensing and relaxing different muscle groups, can help reduce physical tension and ease the transition into sleep. A 2011 study published in the Journal of Sleep Research found that progressive muscle relaxation improved both sleep quality and sleep onset for individuals suffering from anxiety-related sleep disturbances.
Yoga, particularly gentle forms like Hatha yoga, has also been shown to have a positive effect on sleep. A 2013 study published in Alternative Therapies in Health and Medicine found that individuals who practiced yoga regularly reported improved sleep quality, reduced daytime fatigue, and decreased symptoms of insomnia. Yoga combines physical postures, breathing exercises, and meditation to promote both physical and mental relaxation, making it an excellent tool for reducing stress before bed.
Creating a calming bedtime routine that includes these relaxation techniques can further support healthy sleep patterns. Establishing a consistent, calming pre-sleep routine helps signal to the body that it’s time to transition from the day’s activities to restful sleep. A 2019 study published in Sleep Health found that individuals who engaged in calming activities like reading or listening to soothing music before bed had better sleep quality compared to those who spent their evenings engaged in stimulating activities like watching TV or working on a computer.
Additional Preventive Measures
In addition to the strategies above, there are several other preventive measures that can help improve sleep quality and prevent sleep disorders:
-
Limit Stimulants: Avoid consuming caffeine, nicotine, or alcohol in the hours leading up to bedtime, as these substances can interfere with your ability to fall asleep.
-
Exercise Regularly: Regular physical activity can help promote better sleep, but try to avoid vigorous exercise close to bedtime, as it can increase adrenaline levels and make it harder to fall asleep.
-
Eat a Balanced Diet: Certain foods, such as those high in tryptophan (found in turkey, nuts, and dairy), can promote the production of serotonin and melatonin, helping regulate sleep.
In conclusion, preventive measures like creating a sleep-friendly environment, maintaining a consistent sleep schedule, and reducing stress are essential for improving sleep quality and preventing sleep disorders. By taking a proactive approach to sleep hygiene, individuals can reduce the risk of developing chronic sleep problems and enjoy more restorative sleep, leading to better overall health and well-being.
FAQ
What are the most common sleep disorders?
Some of the most common sleep disorders include insomnia, sleep apnea, narcolepsy, restless leg syndrome, and circadian rhythm disorders.
How does light therapy help with sleep disorders?
Light therapy helps regulate the body’s circadian rhythms, improving sleep quality and making it easier to fall asleep and wake up at appropriate times.
What is the role of Luminette in light therapy?
The Luminette is a wearable device that provides light therapy to help reset your body’s internal clock and improve sleep quality. It is particularly useful for people with circadian rhythm disorders.
Can sleep disorders be cured permanently?
While some sleep disorders can be managed effectively with treatment, many may require ongoing management. Lifestyle changes, therapy, and medication can help improve sleep quality.
How do I know if I have a sleep disorder?
If you experience difficulty falling asleep, staying asleep, or excessive daytime fatigue, you may have a sleep disorder. A healthcare professional can help diagnose and recommend treatment options.
Are there natural remedies for sleep disorders besides light therapy?
Yes, natural remedies for sleep disorders can include practices like relaxation techniques, some supplements like melatonin, and improving sleep hygiene.






























 Please note
Please note