Modernit sisustukset käyttävät valoa paljon muuhun kuin näkyvyyteen; valaistus toimii nyt ympäristösignaalina, joka muokkaa huomiota, mielialaa ja ihmisen biologista kelloa. Markkinoilla kuitenkin kaksi hyvin erilaista kategoriaa sekoitetaan usein: koristeellinen tunnelmavalaistus, joka luo ilmapiiriä, ja kliininen valohoito, joka on suunniteltu siirtämään vuorokausirytmiä ja vakauttamaan mielialan fysiologiaa. Markkinointikieli usein hämärtää rajaa, esimerkiksi ”pehmeä iltahohde paremman unen puolesta” tai ”energisoiva päivänvalovaikutus”, vaikka laitteesta puuttuisi biologiseen vaikutukseen vaadittu intensiteetti, spektri ja ajoitusprotokollat. Koristeen ja terapian erottaminen ei ole semanttinen pikkuvirhe vaan valohygienian kulmakivi, koska rutiinit joko vahvistavat tervettä unta tai heikentävät sitä huonosti ajoitetun ja riittämättömän valoaltistuksen kautta (Harvard Health, 2023 Czeisler ym., 2019.)
Vastaavasti on tärkeää ymmärtää tarkoitus ja ajoitus. Koristevalo on joustavaa: lämpimät, himmeät valonlähteet illalla vähentävät silmien rasitusta, rentouttavat hermostoa ja tekevät tiloista turvallisia ja intiimejä. Terapeuttinen valo on kurinalaista: korkea valaistusvoimakkuus, sinisellä rikastettu valkoinen valo annetaan pian heräämisen jälkeen melatoniinin estämiseksi, vuorokausirytmin aikaistamiseksi ja aamuvireyden lisäämiseksi. Sama fyysinen ärsyke väärään aikaan voi kääntyä itseään vastaan, koska kirkas, viileä valo myöhään päivällä viivästyttää nukahtamista, siirtää kelloa myöhäisemmäksi ja pirstoo unen rakennetta (Cajochen ym., 2019 Sleep Medicine Reviews, 2022.)
Keskeiset opit: esteettinen valo ei ole terapeuttinen annos; tehokas valohoito kohdistuu ipRGC–SCN-reittiin riittävällä luksilla, spektrillä ja aamun ajoituksella; ja kestävät tulokset riippuvat johdonmukaisesta aamun altistuksesta sekä kirkkaan, lyhytaaltoisen valon hillinnästä illalla (National Sleep Foundation, 2022 Reid et al., 2018.)

Mitä ”Tunnelmavalaistus” Käytännössä Oikeastaan On
Tunnelmavalaistus on tunnepohjaisen suunnittelun väline. Se muokkaa värilämpötilaa, suuntaa ja hajotusta muuttaakseen huoneen tunnelmaa esimerkiksi kodikkaaksi, intiimiksi, leikkisäksi tai moderniksi. Tyypillinen silmien valaistusvoimakkuus on alle 500 luksi, kaukana ulkoilman päivänvalon tasosta ja alle terapeuttisten kynnysten. Lämpimät sävyt noin 2700–3000 K suositaan rentoutumiseen ja nukahtamisen valmisteluun, kun taas kylläiset RGB-kohtaukset tukevat estetiikkaa tai kokemuksellisia vaikutuksia. Havaintohyödyt ovat todellisia, koska vähentynyt karheus ja pehmeämpi kontrasti luovat rauhallisemman ilmapiirin, mutta ne toimivat ensisijaisesti psykologisten kanavien kautta eivätkä vuorokausirytmin fysiologian kautta (Baselin yliopisto, 2020 Harvard Health, 2023.)
Todellisissa kodeissa ja toimistoissa tunnelmavalaistus toimii kerroksena toiminnallisen valaistuksen päällä: pöytävalaisimet, jotka valaisevat seiniä, LED-nauhat, jotka korostavat arkkitehtonisia yksityiskohtia, meripihkanväriset hehkulamput, jotka alentavat vireystilaa oleskelutiloissa, ja älylamput, jotka tallentavat suosikkikohtauksia. Nämä elementit parantavat mukavuutta ja visuaalista ergonomiaa, erityisesti yöllä, kun korkean korreloidun värilämpötilan valo voi tuntua kliiniseltä tai aktivoivalta. Koska intensiteetti on maltillinen ja spektrit usein poikkeavat taivaansinisen alueen valosta, tunnelmavalaistus ei aktivoi verkkokalvon melanopsiinia tarpeeksi siirtääkseen kehon kelloa tai merkittävästi estääkseen melatoniinia. Se täydentää sisustusta; se ei hoida unihäiriöitä (Reid et al., 2018.)
Yleisiä tunnelmavalaistustyyppejä ovat RGB-LED-nauhat ja -paneelit värikohtauksia varten, meripihkanväriset vintage-lamput noin 2200–2400 K, älylamput rentoutusasetuksilla, koristeelliset seinäkynttilät ja lyhdyt, suolalamput sekä pehmeät hajavalaisimet työpöydille.
Tyypilliset tuotteet ja käyttötapaukset
Kotitaloudet käyttävät RGB-nauhoja televisioiden ja sängynpäätyjen takana visuaalisen draaman luomiseksi, meripihkanvärisiä lasilamppuja olohuoneissa häikäisyn vähentämiseksi ja älylamppuja, jotka himmentyvät hitaasti ennen nukkumaanmenoa. Majoitusala käyttää lämpimiä seinävalaisimia ja seinäkynttilöitä ohjatakseen asiakkaita rauhalliseen keskusteluun. Peliasetukset suosivat kylläisiä sävyjä immersioelämyksen lisäämiseksi. Nämä laitteet optimoivat havaintoa, eivät kiertäjäisen rytmin säätelyä, tehden niistä erinomaisia kumppaneita iltarutiineihin, joissa halutaan matalaa vireystilaa (Baselin yliopisto, 2020.)
Käyttötapauksiin kuuluvat lukupaikat 2700 K lampuilla, yöpöydän meripihkanväriset yövalot melatoniinin häiriön minimoimiseksi, lämpimät seinävalaisimet viihtyisiin oleskelutiloihin, RGB-valaistus viihdealueille ja pehmeä käytävävalaistus yöaikaisen häikäisyn vähentämiseksi.
Miksi tunnelmavalaisimet eivät siirrä sisäistä kelloasi
Kiertäjäinen säätely perustuu sisäisesti valolle herkkiin verkkokalvon gangliosoluihin, jotka reagoivat voimakkaasti sinivihreään valoon aallonpituudella noin 460–480 nm, kun sitä annetaan riittävällä intensiteetillä ja biologisesti merkityksellisellä kestolla. Tunnelmavalaisimet epäonnistuvat yleensä vähintään kahdella akselilla: silmään kohdistuva lux-arvo on liian alhainen ja spektriprofiilit on suunniteltu tunnelmaa varten eivätkä melanopista tehokkuutta ajatellen. Ilman annosta, joka merkittävästi stimuloi ipRGC-SCN-reittiä, näet kauniimman huoneen, mutta et aikaista melatoniinin alkamista tai siirrä kehon lämpötilan minimiä aikaisemmaksi. Lyhyesti sanottuna tunnelmavalaisimet muuttavat tuntemustasi huoneesta, eivät fysiologiasi ajanottoa (Cajochen ym., 2019 Czeisler ym., 2019.)
Kliinisen valoterapian perusteet
Kirkasvaloterapia on kliininen protokolla, joka käyttää kontrolloitua korkeatehoista, sinivalkoista valoa vaikuttaakseen kiertorytmin vaiheeseen ja mielialan säätelyyn. Todisteet alkoivat kaamosmasennuksesta ja ovat laajentuneet viivästyneeseen univalverytmin häiriöön, jet lagiin ja tukirooleihin ei-kausiluonteisessa masennuksessa. Oikein ajoitetut aamun sessiot estävät melatoniinia, lisäävät kortisolia sen luonnollisessa huipussa ja aikaistavat vaihetta, parantaen uniaikaa, valppautta ja päivävireyttä (Lam et al., 2016 Lewy et al., 2018.)
Tärkeimpiin parametreihin kuuluvat valaistusvoimakkuus tyypillisesti 2 000–10 000 luksilla silmään, spektri, jossa on vahva melanopinen sisältö, ajoitus noin 30–60 minuuttia heräämisen jälkeen, kesto noin 20–45 minuuttia ja geometria, joka vakauttaa verkkokalvon annoksen ilman häikäisyä. Kun nämä täyttyvät, tulokset ovat luotettavia; kun ne ovat puutteellisia, kuten liian himmeä, liian myöhäinen tai liian lyhyt, hoito ei toimi odotetusti tai jopa viivästyttää kelloa (Sleep Medicine Reviews, 2022 National Sleep Foundation, 2022.)
Kliinisen hygienian tee ja älä: Käytä aamuajoitusta, istu valmistajan määrittämällä etäisyydellä, pidä silmät avoimina ja vilkaise lähteeseen säännöllisesti, ja toista päivittäin. Älä käytä kirkasta terapiavaloa myöhään iltapäivällä tai illalla, älä venytä sessioita korvataksesi menetettyjä päiviä, äläkä oleta, että mielialalamput voivat korvata terapeuttisen annoksen.
Indikaatiot ja todisteiden yleiskatsaus
Indikaatiot sisältävät kaamosmasennuksen, viivästyneen univalverytmin häiriön, kiertotyön ja jet lagin aiheuttaman kiertorytmin epäsäännöllisyyden, kognitiivisen suorituskyvyn tukemisen vähäisen päivänvalon olosuhteissa sekä tukiroolit ei-kausiluonteisessa masennuksessa kliinisen valvonnan alaisena (Lam et al., 2016 Sleep Medicine Reviews, 2022.)
Todisteet osoittavat, että kirkas aamuvalo vähentää masennusoireita SAD:ssa, aikaistaa uniajan DSWPD:ssä noin 1–2 tunnilla ja parantaa valppautta väestöissä, joilla on rajoitettu päivänvalon saanti, kuten toimistotyöntekijät ja korkeilla leveysasteilla asuvat. Vaikutuksen suuruus riippuu noudattamisesta, annoksesta ja myöhäisen illan kirkkaan valon estosta (Lewy et al., 2018 Reid et al., 2018.)
Annosteluparametrit, joilla on todellista merkitystä
Mielialavalaistus vs Terapia: Tärkeä rinnakkainen vertailu
Ennen valopohjaisen rutiinin omaksumista, perusta odotukset objektiivisiin eroihin. Sisustus optimoi tunnelman ja mukavuuden; terapia kohdistuu biologiaan ja ajoitukseen. Alla olevan taulukon lukeminen tarkistuslistana estää väärinymmärryksiä, kuten tyylikkään lampun ostamisen kliiniseen lopputulokseen, jota se ei voi tarjota (Sleep Medicine Reviews, 2022.)
Kriteeri |
Mielialavalaistus (Sisustus) |
Valoterapia (Kliininen) |
Pääasiallinen tarkoitus |
Ilmapiiri ja visuaalinen mukavuus |
Kiertorytmin vaiheensiirto ja mielialan säätely |
Tyypillinen valaistusvoimakkuus |
Alle 500 luksilla silmässä |
2 000–10 000 luksilla silmässä |
Spektri |
Lämmin tai RGB, esteettinen |
Sinisellä rikastettu valkoinen, melanopisesti tehokas |
Käytön ajoitus |
Joustava, usein illalla |
Tiukasti aamulla heräämisen jälkeen |
Odotettu tulos |
Koettu rentoutuminen ja miellyttävyys |
Melatoniinin estäminen, vaiheensiirto eteenpäin, vireystila |
Protokolla |
Ei mitään, kohtauspohjainen |
20–45 min päivittäin, toistettava geometria |
Taulukon tulkinta: Mitä kukin rivi tarkoittaa
Miten valo kommunikoi aivojen kanssa
Ihmisen vuorokausirytmiä säätelee suprachiasmaattisen ytimen mestarikellosepä, joka synkronoituu päivittäin verkkokalvon valosignaalien avulla. Erityiset sisäisesti valolle herkät verkkokalvon gangliosolut, jotka sisältävät melanopsiinia, projisoivat retinohypotalamuksen radan kautta suprachiasmaattiseen ytimeen, joka koordinoi hormonirytmejä kuten melatoniinia ja kortisolia, kehon peruslämpötilaa ja univalvetilaa. Aamun sinisellä rikastettu valo nopeuttaa kelloa vaiheensiirtona eteenpäin, kun taas myöhäinen iltasininen valo viivästyttää sitä, siirtäen unta myöhemmäksi ja vähentäen hitaiden aaltovaiheiden konsolidointia (Czeisler ym., 2019 Cajochen ym., 2019.)
Käytännön seuraus on, että annos ilman ajoitusta on tehoton. Kymmenen minuuttia 10 000 luksilla keskipäivällä ei vastaa 30–40 minuuttia ensimmäisen tunnin aikana heräämisen jälkeen. Samoin johdonmukainen iltavalaistuksen himmennys lyhytaaltoisesta sisällöstä on voiman moninkertaistaja, koska se suojaa aamun sessioiden hyödyt sallimalla melatoniinin erityksen alkaa aikataulun mukaisesti. Monet kotitaloudet pyyhkivät tiedostamattaan aamun hyödyt pois käyttämällä kirkasta työvaloa tai näyttöjä auringonlaskun jälkeen (Reid et al., 2018 Harvard Health, 2023.)
Reitin vaiheet yksinkertaistettuna: 1) sinisellä rikastetut fotonit saavuttavat ipRGC:t, 2) signaalit kulkevat suprachiasmaattiseen tumakkeeseen, 3) kello siirtää geeniekspression ajoitusta, 4) melatoniinin esto ja kortisolin kohdistus tapahtuvat, 5) aikaisempi uneliaisuus ja parantunut aamuvireys seuraavat.
ipRGC:n ja SCN:n välinen reitti yksinkertaistettuna
Ajattele ipRGC-soluja valon aikahavaitsijoina. Ne eivät muodosta kuvia, vaan raportoivat valon päivän aivoille. Riittävällä aamun ärsykkeellä sisäinen tahdistin kohdistaa solukellot koko kehossa keskus- ja ääreisrytmittäytymisen mukaisesti, vakauttaen ruokahalun rytmit, lämpötilan minimin ja kognitiiviset huiput. Riittämätön aamun ärsyke aiheuttaa sisäistä harhaa, joka kasaantuu myöhäisiin nukkumaanmenoihin, vaikeisiin heräämisiin ja sosiaaliseen jetlagiini (Czeisler ym., 2019 Roenneberg et al., 2012.)
Ajoitusikkunat: aamun aikaistus vs illan viivästys
Kuinka tunnistaa aito terapiaväline ja välttää näennäiset vastaavat
Kuluttajamarkkinoilla on monia hyvinvointilamppuja, jotka esittävät terapeuttisia väitteitä. Aito terapiaväline on tarkka annoksesta, geometriasta, turvallisuudesta ja ajoituksesta. Käytä tätä tarkistuslistaa suodattimena ennen ostoa ja vaatimustenmukaisuustyökaluna jälkeenpäin.
Tarkistuslista vaatimuksista: silmien tasolla vähintään 2 000 luksia määritellyllä etäisyydellä ja kulmalla, sinisellä rikastettu valkoinen tai melanopisesti tehokas spektri ja UV-vapaa lähtö, aamun ajoitusohjeistus sessiokeston kanssa, vakaa geometria silmänpohjan annoksen varmistamiseksi, turvallisuusohjeet mukaan lukien häikäisyn hallinta ja silmävaroitukset, sertifiointi kuten CE tai FDA-luokka soveltuvin osin, sekä käyttäjäohjeistus annoksen asteittaisesta vähentämisestä tai ohjeet ohitetun päivän käsittelyyn (National Sleep Foundation, 2022 Sleep Medicine Reviews, 2022.)
Markkinoinnin punaiset liput sisältävät ilmaisuja kuten ”lisää energiaa” ilman luksarvoa tai etäisyyttä, RGB-terapiatilat, illan unta parantavat kirkkaan valkoiset esiasetukset, turvallisuus- tai sertifiointitietojen puute, koristeelliset kuvat ilman protokollakieltä ja epämääräinen ajoitus kuten ”käytä milloin tahansa.” Nämä merkit viittaavat yleensä sisustukseen, joka naamioituu terapiaksi (Reid et al., 2018.)
Toimivat rutiinit: Aamun valon sisällyttäminen arkeen
Suunnittele protokollasi heräämisesi ympärille, ei pelkästään kellonajan mukaan. Paras käytäntö on aloittaa 30–45 minuutin kuluessa heräämisestä, yhdistää sessio rutiininomaiseen ankkuriin, kuten aamiaiseen tai sähköpostin lajitteluun, ja pitää kesto tasaisena 20–40 minuutissa. Vahvista lyhyellä ulkoilman valotauolla, jos mahdollista, koska jopa varjostettu päivänvalo tarjoaa melanopista sisältöä, jota ei ole saatavilla sisätiloissa. Illalla himmennä lämpimäksi ja katkaise suorat sinisen valon lähteet 1–2 tuntia ennen nukkumaanmenoa. Nämä kaksi toimenpidettä, aamun valon lataus ja illan suojaus, tuottavat suhteettoman suuria hyötyjä vaivaan nähden (National Sleep Foundation, 2022 Harvard Health, 2023.)
7 vaiheen aloitussuunnitelma yhdelle viikolle: 1) kiinnitä heräämisaika plus- tai miinus 15 minuutin ikkunalla, 2) aloita valohoito 30–45 minuutin sisällä ja tee 25–35 minuuttia per istunto, 3) pidä laite määritetyssä etäisyydessä ja kulmassa ja pidä silmät luonnollisesti avoinna, 4) yhdistä rutiinitehtävään noudattamisen automatisoimiseksi, 5) lisää aamupäivällä 5–10 minuutin ulkovalotauko, jos mahdollista, 6) auringonlaskun jälkeen käytä lämpimiä ja himmeitä kohtauksia ja rajoita näyttöjä, 7) viikko viikolta siirrä nukkumaanmenoaikaa 10–15 minuuttia aikaisemmaksi unenpaineen edetessä (Roenneberg et al., 2012 Reid et al., 2018.)
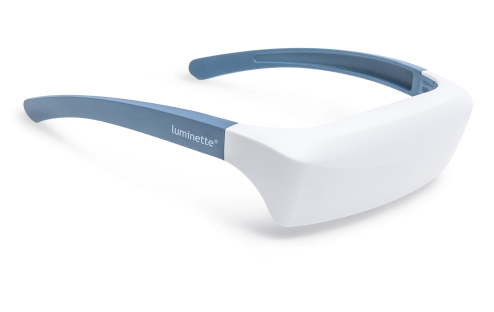
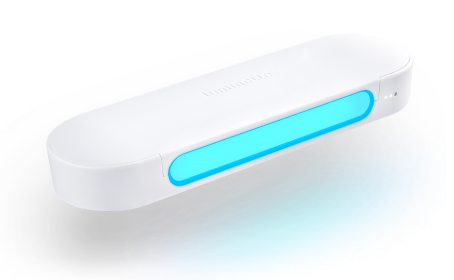
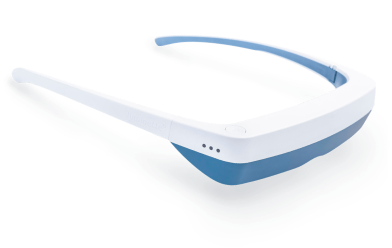
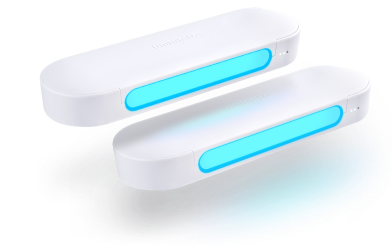
Kannettava valohoito: Miksi noudattaminen muuttaa kaiken
Paikallaan olevat valolaatikot perustuvat näyttöön, mutta ovat ergonomisesti jäykkiä, koska istut paikallasi, kohtaat paneelin ja odotat. Vilkkaissa kodeissa ja nuorten keskuudessa hoidon noudattaminen heikkenee, koska hoito kilpailee aamun logistiikan kanssa. Kannettavat ratkaisut ratkaisevat geometriaongelman tuomalla valonlähteen silmien lähelle hallitussa kulmassa samalla kun liikkuvuus säilyy, mikä muuttaa hoitoajat käsivapaaksi rutiiniajaksi. Parempi noudattaminen ei ole vain mukavuustekijä, koska se usein erottaa tilastolliset ja kliiniset vaikutuskoot (Sleep Medicine Reviews, 2022.)
Kannettavat laitteet vähentävät myös sijoitusvirheitä. Visiirityylisellä optiikalla melanopinen annos pysyy vakaana luonnollisten päänliikkeiden aikana. Käyttäjät voivat valmistaa aamiaista, pakata laukkua tai lukea sähköpostia ilman jatkuvaa paneelin uudelleen kohdistamista. Turvallisuus on varmistettu häikäisysuojatuilla optiikoilla, UV-vapailla LED-valoilla ja maltillisella valaistuksella, kuten 2 000 luksilla silmän tasolla paneelin huippuarvojen sijaan. Tulosten kannalta samankaltaiset vaiheensiirtymät paremmalla päivittäisellä johdonmukaisuudella voivat ylittää teoreettisesti korkeamman luksin, jota käyttäjät eivät todellisuudessa saavuta (Reid et al., 2018 Harvard Health, 2023.)
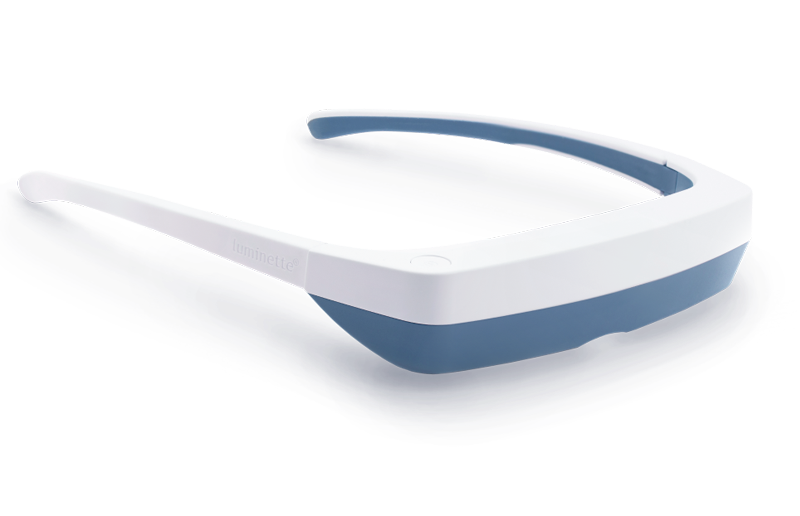
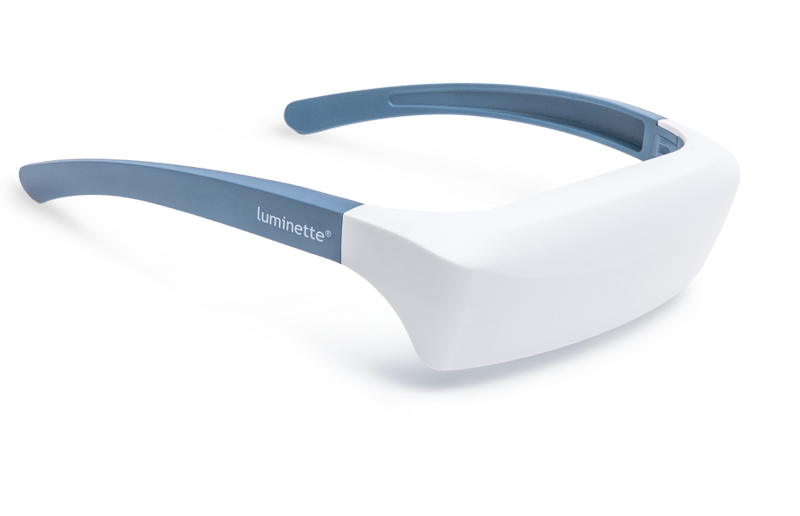
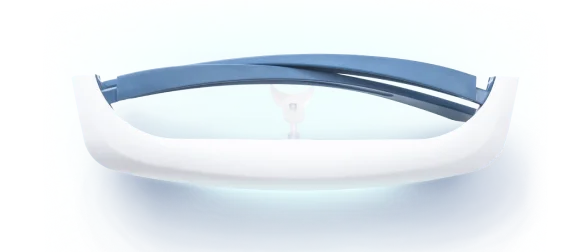
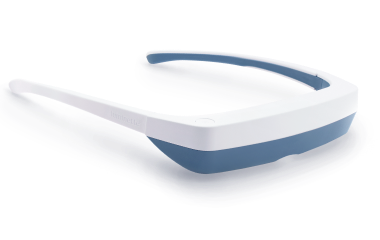
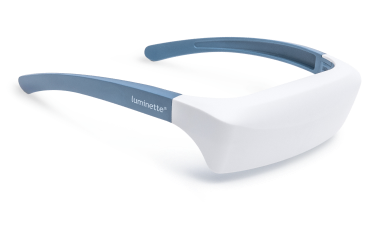
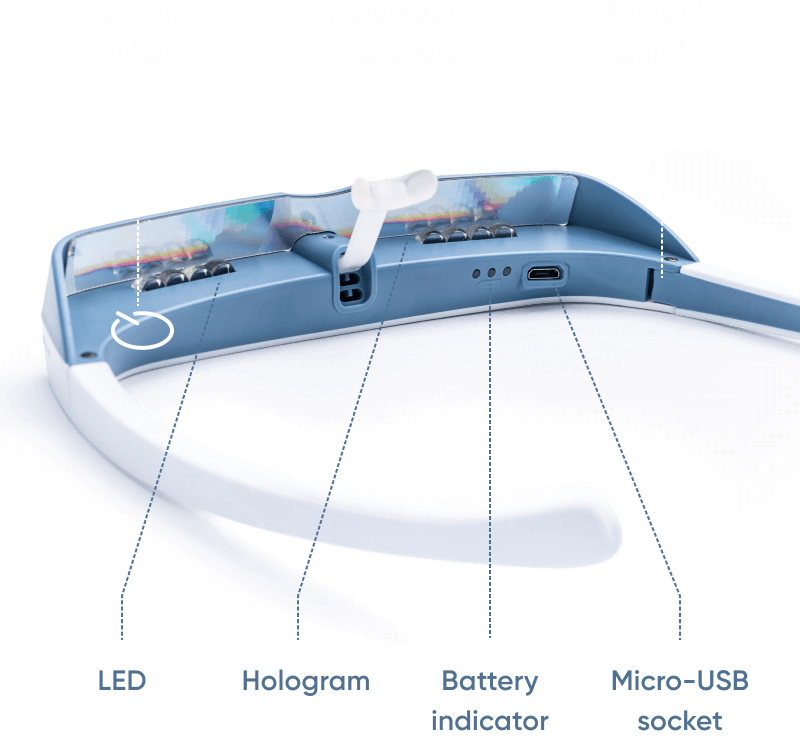
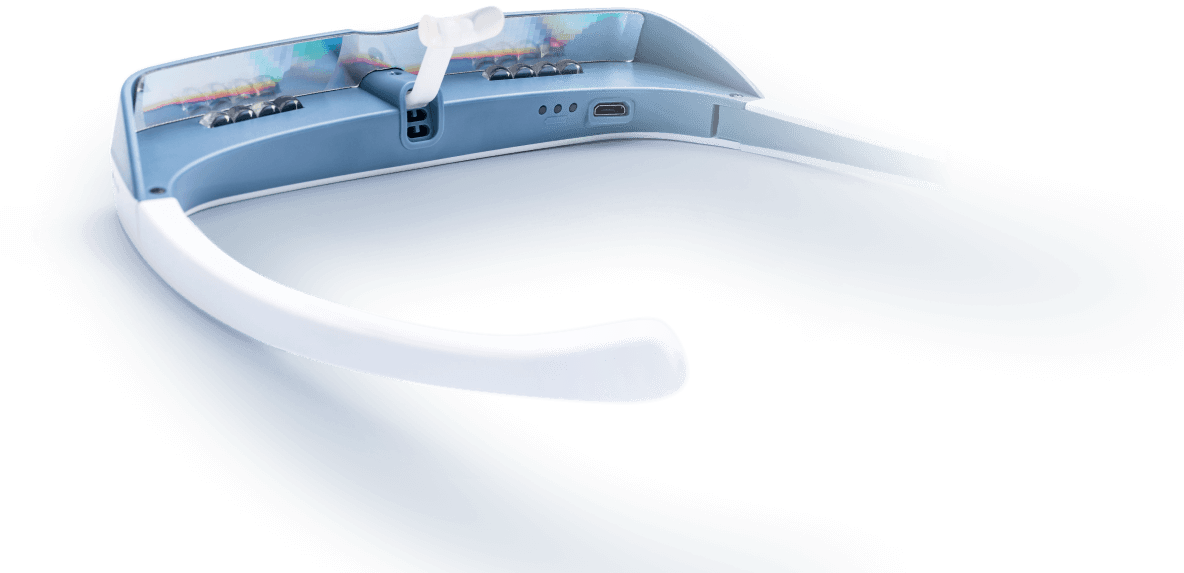
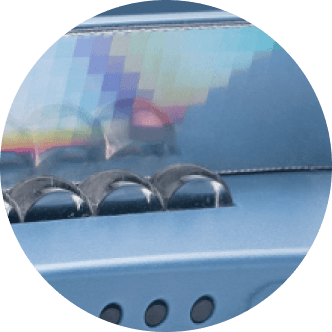
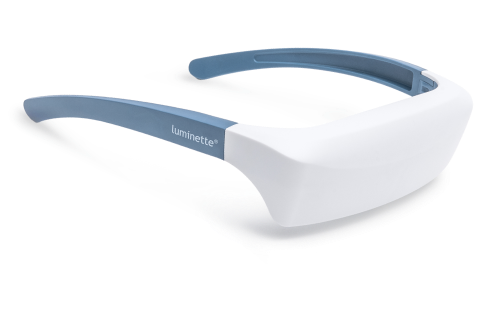
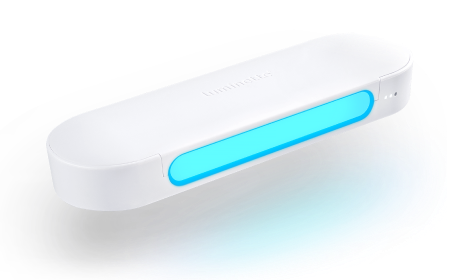
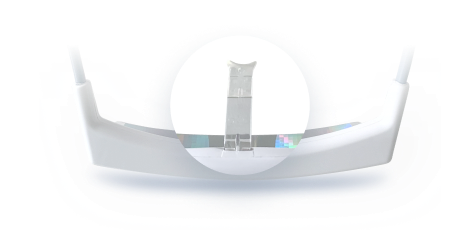
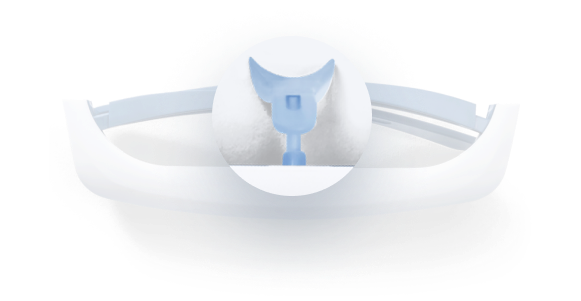
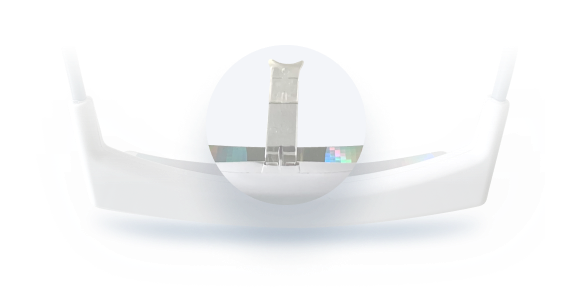
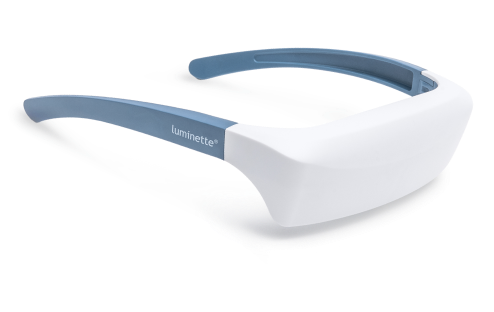
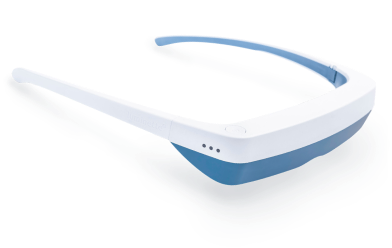
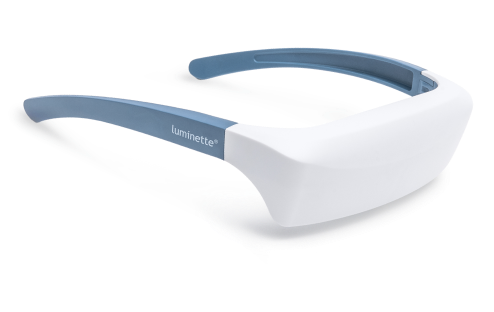
Esimerkki: Luminette 3 aamun sessioihin
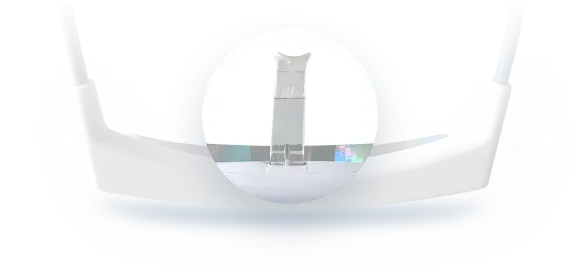
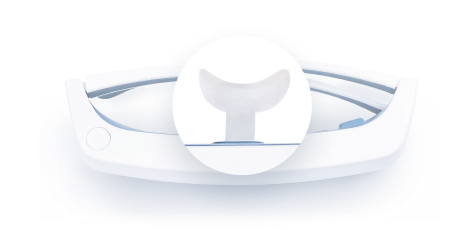
Optiikka ja annoksen toimitus. Luminette 3 käyttää yläasennettua LED-matriisia ja diffraktiolinssejä, jotka projisoivat sinivaloa rikastettua valkoista valoa alaspäin kohti alempaa verkkokalvoa, jossa melanopsiinipitoiset ipRGC-solut reagoivat tiheästi. Suunnittelu pitää valonsäteen pois keskeiseltä näkökentältä, säilyttäen näkökentän reuna-alueet ja minimoiden häikäisyn samalla kun se toimittaa noin 2 000 luksin annoksen silmälle, mikä on kliinisesti merkittävä aamun annos 20–45 minuutissa. Geometria on kiinteä kehyksen avulla, mikä vähentää käyttäjävirheitä ja parantaa toistettavuutta.
Käytettävyys ja turvallisuus. Koska näkö pysyy esteettömänä, käyttäjät voivat liikkua vapaasti. LEDit ovat UV-vapaita, optinen rakenne on säädetty mukavuuden takaamiseksi, ja ohjeistus korostaa aamun ajoitusta. Tämä ratkaisee valoterapian suurimman esteen, eli hoidon noudattamisen, vaarantamatta biologista tavoitetta. Varhaiset kokeet, joissa kannettava toimitus verrattiin paikallisiin laitteisiin, raportoivat vertailukelpoisia vaiheensiirtoja paremmalla noudattamisella ja käyttäjätyytyväisyydellä, erityisesti nuorilla ja kiireisillä ammattilaisilla (Rüger et al., 2020 Sleep Medicine Reviews, 2022.)
Tekstimuistiona pyynnöstä: Saatavilla on myös kannettava muoto — Luminette 3 — säännöllisiin aamun valosessioihin, joka selittää valon kompensaation luonnollisesti.
Keskeiset ominaisuudet yhdellä silmäyksellä sisältävät kontrolloidun 2 000 luksin silmälle, sinivaloa rikastetun valkoisen spektrin, visiirin geometrian, joka kohdistaa valon alemmalle verkkokalvolle, UV-vapaat ja häikäisysuojatut optiikat, 20–45 minuutin aamuprotokollan ja liikkuvuuden session aikana.
Kliiniset ja psykologiset odotettavissa olevat tulokset
Oikein käytettynä aamun valoterapia osoittaa yhteneviä hyötyjä unen ajoituksessa, vireystilassa ja mielialassa. Kaamosmasennuksessa oireiden väheneminen kahden viikon sisällä on hyvin dokumentoitu. Viivästyneessä univalverytmin häiriössä vaiheensiirrot noin 1–2 tuntia ovat tyypillisiä, usein aikaisemman nukahtamisen ja helpompien heräämisaikojen kanssa. Toimistotyöntekijät ja korkeiden leveysasteiden asukkaat raportoivat parantunutta valppautta ja vähentynyttä aamupäivän uneliaisuutta. Vaikutukset korostuvat säännöllisyydellä, oikealla ajoituksella ja iltavalaistuksen kurinalaisuudella (Lam et al., 2016 Lewy et al., 2018 Reid et al., 2018.)
Tulokset sisältävät aikaisemman nukahtamisen ja heräämisen, vähentyneen päiväunen tarpeen, parantuneen reaktioajan ja työmuistin, mielialan vakaantumisen talvikuukausina, paremman kortisolihuipun ajoittumisen aamuun sekä koetun unen laadun paranemisen.
Rajoitukset, turvallisuus ja oikeat käyttöajat
Valoterapia on yleisesti turvallista, mutta ei ajasta riippumatonta. Myöhäisillan sessiot voivat viivästyttää unta, pitkät altistukset voivat aiheuttaa ohimenevää päänsärkyä tai silmien rasitusta, ja kaksisuuntaisen mielialahäiriön tai tiettyjen silmäsairauksien kanssa elävät tarvitsevat lääketieteellistä ohjausta haitallisten reaktioiden välttämiseksi. Kohtele valoterapiaa kuten mitä tahansa hoitoa: seuraa vasteita, säädä kestoa suositelluissa rajoissa ja priorisoi aamun aikavälit vaiheensiirron edistämiseksi samalla kun suojaat iltoja kirkkaalta sinivaloiselta valolta (American Psychiatric Association, 2021 Cajochen ym., 2019.)
Käytä varoen -tarkistuslista sisältää historian maniasta tai hypomaniasta, verkkokalvosairaudesta tai äskettäisestä silmäleikkauksesta, kirkkaan valon laukaisemasta migreenistä, hallitsemattomasta ahdistuksesta aktivoivien ärsykkeiden yhteydessä ja valolle herkistävien lääkkeiden käytöstä. Konsultointia tarvitaan, jos ilmenee levottomuutta tai unettomuutta aamun ajoituksesta huolimatta, jatkuvia päänsärkyjä tai näköhäiriöitä, joita ei helpota etäisyyden tai kulman säätö.
Valon terveellisten tilojen suunnittelu: Päivittäinen valaistussuunnitelma
Yhdistä sisustus ja terapia päivänajan mukaan. Käytä aamun terapeuttista altistusta kellon asettamiseen, ylläpidä kirkasta neutraalia työvaloa työaikana ja himmennä lämpimiin hajavaloihin auringonlaskun jälkeen. Tätä lähestymistapaa, jota kutsutaan vuorokausikerrostukseksi, käytetään tunnelman ja fysiologian yhteensovittamiseen, jolloin tunnelmavalot loistavat iltaisen rauhan aikaan ilman, että ne korvaavat kliinistä aamudoseerausta.
Päivän aikataulutaulukko:
Aikajakso |
Tavoite |
Valotyyppi |
Esimerkki |
Aamu, 0–60 min heräämisen jälkeen |
Vaiheen aikaistaminen ja vireystila |
Valoterapia tai sinisellä valolla rikastettu valkoinen, korkea luksitaso |
Luminette 3 -istunto 20–40 min |
Päivätyö |
Jatkuva valppaus |
Neutraali tai viileä työvalo, kohtalainen tai kirkas |
4000–5000 K työpöydän valaistus, päivänvalotauot |
Ilta, 2 tuntia ennen nukkumaanmenoa |
Melatoniinisuoja |
Lämmin, himmeä, hajavalo |
2200–2700 K lamput, vähäinen häikäisy, ei kirkkaita näyttöjä |
Mihin ala on menossa: personoitu, adaptiivinen valaistus
Seuraava aalto on personoitu fotobiologia, jossa järjestelmät mukauttavat spektriä ja intensiteettiä kronotyypin, univelan ja vuodenajan mukaan. AI-ohjatut valaisimet ja kannettavat laitteet koordinoivat aikatauluja varmistaen vahvan aamun melanopisen annoksen ja vähäisen ilta-altistuksen. Integrointi unenseurantalaitteiden ja ympäristön antureiden kanssa mahdollistaa suljetun silmukan ohjauksen, joka mittaa, mukauttaa ja säätelee (Nature Electronics, 2023.)
Nousevia trendejä ovat adaptiiviset vuorokausirytmit, melanopista tietoisuutta lisäävät spesifikaatiot, kannettavien ja kotien synkronointi, työpaikkojen päivänvalon kompensointi sekä annosteluohjelmat käyttäytymisen ohjauksella.
Yhteenveto ja käytännön vinkit
Sisustus- ja hoitovalot täydentävät toisiaan, eivät ole toistensa korvikkeita. Käytä tunnelmavalaistusta tilan tunnelman muokkaamiseen ja aamun valohoitoa biologisen kellon säätelyyn. Kiinnitä rutiinit heräämiseen, suojaa illat ja valitse laitteet, jotka ilmoittavat selvästi luksin, ajoituksen, spektrin ja geometrian.
Seuraavat askeleet sisältävät varmennetun hoitomuodon valinnan, 20–40 minuutin aamuharjoituksen aloittamisen 30–45 minuutin sisällä heräämisestä, iltavalaistuksen tarkistamisen lämpimäksi ja himmeäksi pitämiseksi, lyhyiden päivänvalotaukojen lisäämisen sekä unen alkamisen ja heräämisen seurannan viikoittain vaiheen edistymisen varmistamiseksi.
UKK
Voivatko tunnelmavalot korvata valohoidon?
Ei, niiden valaistusvoimakkuus on alle 500 luks ja spektri on suunniteltu tunnelmaan, ei vuorokausirytmin säätelyyn. Terapiassa tarvitaan vähintään 2 000 luksia silmään ja aamun ajoitus
Kuinka pitkä hoitokerran tulisi olla?
Useimmat protokollat suosittelevat 20–40 minuuttia ensimmäisen tunnin aikana heräämisen jälkeen; johdonmukaisuus on tärkeämpää kuin maksimaalinen luksus
Onko Luminette 3 turvallinen päivittäiseen käyttöön?
aamun hoitokerrat; käyttäjät säilyttävät liikkuvuutensa, mikä parantaa sitoutumista
Toimivatko älylamput päivänvalotilassa?
Vain jos ne tuottavat terapeuttista luksusta silmään ja niitä käytetään aamulla protokollan mukaisesti; useimmat sisustuslamput ovat liian himmeitä
Mitä jos tunnen oloni levottomaksi yöllä?
Tarkista iltavalaistus, vähennä kirkasta tai sinistä valoa 1–2 tuntia ennen nukkumaanmenoa, äläkä käytä terapiakertoja myöhään illalla































 Huomioithan
Huomioithan